[ edit: I have gotten an ear infection diagnosis and a prescription for antibiotics as of 26 June 2025, [ see comment ] edit 2: as of 5 July 2025, I now think this is probably actually cancer, [ see Tweet ] edit 3: as of 19 July 2025, ehhh could be cancer, could be autoimmune, could be atypical infection, I really have no idea, [ see update Tweet ] edit 4: as of July 22 2025, the swelling has reduced drastically [ probably from the recovery from infection ] and I got a CT scan result saying I had left-lateralized vestibular labyrinth dehiscence [ SCDS, IIUC ], and I suspect it’s actually bilateral SCDS, which is simultaneously causing the vestibular dysfunction directly and causing the ETD via progressive fluid edema ] edit 5 [ circa August 6, 2025 ]: I’ve narrowed it down to almost-certain [ bilateral perilymphatic fistula ] which is just a third window opening directly into your middle ear, and now I’ve got to get it operated on to prevent meningitis edit 6 [ September 23, 2025 ]: Yeah, no, it was a bacterial infection, localized to the place in my Eustachian tubes where I thought it was, after all. It wasn’t cured by the doxycycline or azithromycin because it’s an incredibly antibiotic-resistant staph infection. I ultimately discovered it because it started repeatedly spreading to my skin and eyes, and didn’t respond to antibiotics there, either. It’s showing no response to doxycycline at this point, low response to mupirocin and sulfamethoxazole/trimethoprim, so I’m going to go see what the doctor thinks now. I still haven’t tried a beta-lactam because no one will let me. edit 7 [ September 29, 2025 ]: Have now been on augmentin [ amoxicillin + clauvanate ] for 4.5 days, to no apparent effect. ChatGPT says it’s probably either in my neurons [ which I doubt ] or in a biofilm in my Eustachian tubes [ which seems plausible ] or in my cells. With 4 outbreaks from the initial site over the past year and a half, each more severe than the last, it’s a shame I’m having trouble getting in with a specialist. ]
I have what I think is a chronic inner ear infection. Since March of 2021, I’ve had subjective obstructive Eustachian tube dysfunction in my right ear, as well as oculomotor problems that as far as I can tell must be caused by some kind of inflammation in my semicircular canals. [ The vestibular problem was confirmed by a videonystagmography, but I moved cities before I could follow up with the ENT who ordered the test. ]
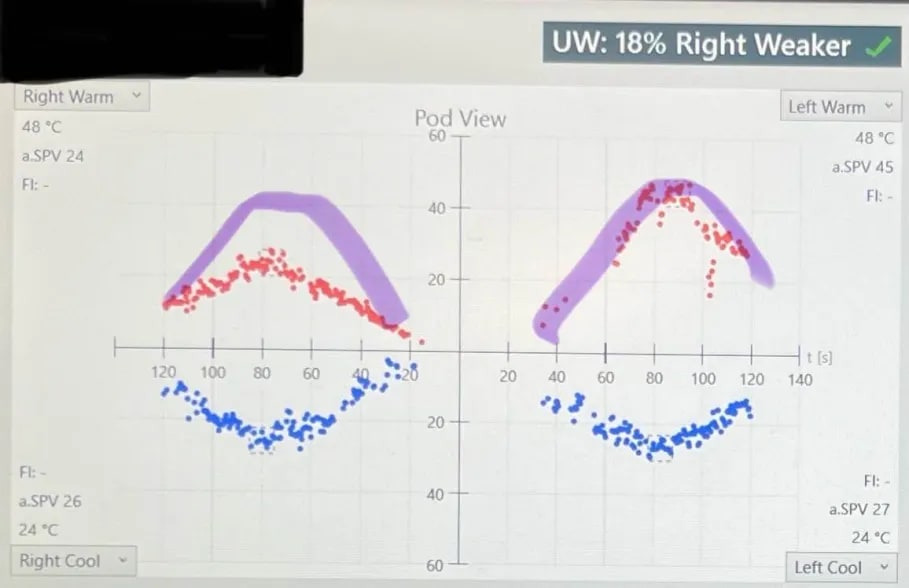
[ Best photo I have left of my VNG results, from June of 2024. The red scatterplots show my labyrinths’ response to warm water, blue cold. The purple highlights [ drawn by me after the tester’s description ] show where my vestibular heat reflex should be; the red parts of the scatterplot show that at the time my left oculomotor reflex was OK but my right was deficient. ]
[ illustration of how the 2 oculomotor reflexes of each eye rely differentially on input from the semicircular canals of each ear, which can be tested with a caloric reflex test [ part of my VNG ] -- the rapid nystagmus to the right side is simulated by application of warm water to the right eardrum, while the slow nystagmus to the left side is simulated by application of cold water to the right eardrum ]
In July of 2024 the problem spread to my left ear. I’ve gone to about 8 medical professionals about it, and they’ve consistently prescribed Flonase/Nasacort and otherwise refused to treat it.
The Flonase/Nasacort does anything [ Nasacort works better ], but since March of 2025 [ when the dizziness had gotten really bad and I decided I’d Try Anything ] I’ve found that eating 3-4 cloves of strong garlic a day, plus Nasacort, works vastly better than that.
Since garlic is supposed to be an antibiotic as well as an anti-inflammatory agent, the garlic working so well [ plus reading up on the common causes of ETD that has my symptom profile ] made me suspect it was an infection. I tried ordering ofloxacin from TelyRx and it seemed to help a little but didn’t end up curing the problem, and it rebounded when I ran out of ofloxacin. I’d been worried this would happen. Unfortunately ofloxacin is centrally for when your eardrums are perforated, so the solution can actually penetrate into the inner ear cavity. My eardrums aren’t perforated, and actually look normal to otoscopy most of the time, which is part of why I can’t get treated. I tried taking about 5 leftover doses of very-high-dose amoxicillin and that seemed to help even more but frustratingly I only had a few doses and can’t get more [ the course of amoxicillin was about 20 pills ].
I would write off the apparent partial effectiveness of antibiotics as placebo, especially given that I’ve seen 8 doctors and none has brought up the possibility of an infection. But this spring, I got a fairly bad bacterial skin infection [ a coworker said it looked like I’d fallen off a bike ]. I know it was bacterial because it responded very slowly to copious amounts of Neosporin patiently, meticulously applied over the course of several weeks. In the middle of that, hoping to get something stronger that would work faster, I saw a doctor—who was overwhelmingly confident it looked fungal, and prescribed antifungals. I thought “I’ve had fungal infections before, and it doesn’t really look like that; also, the Neosporin is working really slowly and I’m having to use a lot, but it does appear to be working”. I didn’t take the antifungals and kept using the Neosporin; a week or so later the infection was gone. That shifted my priors both about [1] how good doctors are at clocking baterial infections, and [2] how patient one may have to be with antibiotics.
I’ve thought about doing self-myringotomy in the hopes that giving the fluid an opportunity to drain will cure me; since realizing some of the inflammation must actually be in my labyrinth, to be causing the balance problem, I’m somewhat glad I didn’t try this—at least not without having some ofloxacin on hand—because I doubt that draining alone would solve a labyrinth infection.
I tried using diluted garlic juice as a nasal spray a couple times in May [ your Eustachian tubes connect to your the upper parts of your nasal cavity ]. That seemed to work better than just eating the garlic, but I stopped for fear that the sugar from the garlic juice would sit in my sinuses and cause worse problems.
IIRC I was prescribed a less-than-strong oral antibiotic when the problem started in 2021, but I don’t remember for sure, and I definitely don’t remember if I finished the course. If I did take one, I know it didn’t do anything perceptible. That’s part of why I’ve been hesitant to expend marginal effort obtaining less-than-strong oral antibiotics. If I currently had the money, I’d try ordering strong oral antibiotics from an online pharmacy now; unfortunately, I don’t.
Other than garlic, are there any ways known to LessWrongers of killing bacteria in your inner ears which don’t require a prescription or much money?
I do not know real medical answers to this question. However I have some out-there ideas which could be tried in a way with low risk of making things worse, and some small chance of making things better.
First the worst idea—labyrinthitis is commonly diagnosed by MRI. It’s not cheap—probably costs a couple thousand bucks—but you can get an elective MRI of your head if you really want to see what’s going on in there. That’s not a great suggestion for your case because you’re looking for cheap. But if you get imaging on your own and it shows abnormalities, it could be a good lever for demanding that doctors take you seriously.
Second, consider simulating fever. Some bacteria which like normal body temps stop working right at higher temps that are still low enough not to damage the human. If you have no other contraindications to spending as long as you can tolerate in a sauna as frequently as you can for awhile, it could be worth a try. Just be careful to know the signs that you’re getting other harm from excess heat, and cut back if you notice them.
Third, have you noticed any change in symptoms when taking antihistamines for other reasons? I agree that bacterial infection is the likeliest cause, but there’s some chance that inflammation mimicking infection can be due to inappropriate immune response to stimuli that would be harmless otherwise. If you’re not already on antihistamines for allergies and you have no known reactions to them, it could be a good data point to determine whether OTCs like cetirizine make any difference in subjective symptoms.
Fourth and perhaps silliest, have you tried reframing the “getting doctors to take this problem seriously” as a social engineering challenge, and prompted Claude (preferably Opus) to strategize with you for how to tell the truth from the specific angle that causes medical professionals to pay attention? You shouldn’t have to do this, but the medical system is a mess, and roleplaying your doctor conversations with a bot who can highlight anything you say that decreases your credibility from a health care provider’s perspective may help you change your interactions with them in a way that changes the outcomes.
Ha, I’ve been trying to get my head scanned for four years. Haven’t even come close to getting anyone to take me that seriously. Thank you, though.
. . . Huh, that is a new one to me, thanks! I’ve been hanging out in the heat recently, so that’s convenient. I’ll see if it improves anything.
I’m actually taking certrizine, too, because I was prescribed that as well [ 80% of the doctors insisted it had to be allergies [ even though I don’t have allergies ] or else neurological [ makes little sense IMO ] ]. If the certrizine has an effect, it’s smaller than the effect of the antibiotics, garlic, and steroids.
This suggestion makes a lot of sense, thank you. Idk if you read either of my accounts of what went wrong [ Part 1 [google doc] ], [ Part 2 [blog post] ], but I [ perhaps arrogantly ] pride myself that I’m better at this than even Claude, for the moment.
[ These seem like real medical answers to me. ]
Try it anyways. A quick grep in the links you provided suggests there may be some tricks like specifically requesting the differential diagnoses that you may not yet be using (or you’re using them and not mentioning it, can’t tell from here). From my perspective, the “Haven’t even come close to getting anyone to take me that seriously” earlier in your post suggests that more dakka in the social engineering for being taken seriously department may still be appropriate.
Getting a referral may be harder than pursuing the options for it which are available without a referral. It’s doable, albeit expensive and annoying, without a doctor’s recommendation for it.
If certrizine is the only antihistamine you’ve tried, it may be worth cycling through all available OTC alternatives to it while carefully tracking symptoms before ruling out the whole class.
I don’t know what you mean by “specifically requesting the differential diagnoses”. Care to elaborate?
I just had a conversation with an urgent care doc. I told the office I had a new ear infection, so they wouldn’t look at my previous doctor’s notes saying I’d been “somatizing” the ETD, and in the hopes that letting them come to the conclusion themselves would prevent them from having an allergic reaction to a patient’s “self-diagnosis”.
That worked, insofar as the doctor said he saw inflammation in my nasal passages and lymph nodes that looked like ETD. He explained what that was, and said I should try a nasal steroid. I said I’d tried two kinds [ Flonase and Nasacort ] and I’d been taking them for seven months, and the problem just kept getting worse. He said I should try a third kind of nasal steroid. I asked if I could try an antibiotic. He said no, he hadn’t seen any signs of infection, and thus he couldn’t conscion the risk of antibiotic resistance. I begged as sanely-sounding as I could. I said “I don’t have allergies [ that could be causing the ETD ]”, but he didn’t seem interested in determining the cause of the ETD in the first place. He said no three times to my request to try an antibiotic, and repeatedly said “Steroids are the treatment for ETD”.
I now have a follow-up with my new GP on Thursday. If you know magic words I can say to make that go better, I give you the floor.
I genuinely do not have the money at the moment to get my head scanned or pursue other options without a referral, unfortunately.
asking about differential diagnoses is the doctor-ese way of saying “ok if it’s not what you think, what else are we considering as possible explanations?” which opens a conversation about whether it’s appropriate to also test for those alternatives. Differentials should include the unlikely stuff as well as the likely stuff, and using the professional terminology can signal that you’re capable of understanding that it’s probably a likely thing but could be an unlikely one.
and if you end up in that same conversation about “no signs of infection”, definitely inquire what signs would be externally perceptible. had he been able to actually examine the affected tissue and culture for bacteria, or was he just guessing?
No tissue samples, just external examination. Not even bothering to guess at a cause. “ETD → use steroids to treat”.
If the new GP acknowledges that I have signs of ETD and that it must be caused by something, and that something is probably not allergies [ otherwise the steroids plus azelastine plus certrizine would likely have done anything long-term, and/or I would have any other signs of seasonal allergies to speak of ], that’ll be mission accomplished. So I’m trying to brainstorm ways to force him to acknowledge that syndromes have causes, which is not a standard most doctors I’ve ever talked with in this great state of Iowa have met.
I hope it went ok!
Update: The new GP took one look in my ear and said, and I quote, “You have a lot of . . . infection!”
And was baffled that urgent care hadn’t given me antibiotics.
I imagine it had gotten significantly worse over those few days [ it had subjectively ], as I hadn’t been able to stay supplied with garlic.
I’m now on doxycycline 200mg/day; Google says ear infections are usually caused by Streptococcus pneumoniae, and that this strain in America is resistant to tetracyclines around 1⁄5 of the time. But new GP said if it didn’t work to come back and he’d try something else.
So barring further complications I seem to finally be in the clear.
New doc has been in the area for a while but doesn’t look/talk like he’s from around here; I would hazard a guess that’s why he was a lucky roll.